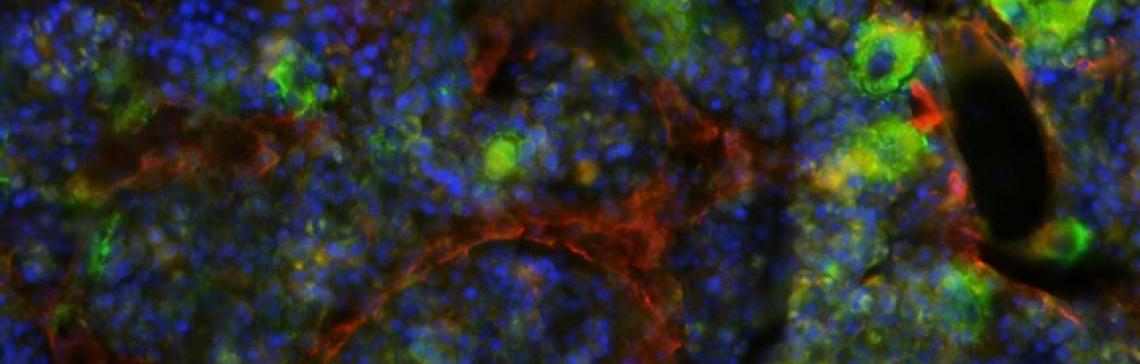
People produce more than a trillion new blood cells every day. Blood cells (red cells, white cells, and platelets) come from blood stem cells (aka, hematopoietic stem cells or HSCs) that normally live in the bone marrow at the center of your bones. Despite the vast number of blood cells produced each day, each person only has a few tens of thousands of blood stem cells that serve us throughout life.
Blood stem cells can be transplanted from one person to another if the immune system of the stem cell donor and the person being transplanted (recipient) are compatible. This approach was originally done using bone marrow and, for this reason, it was called a “bone marrow transplant” or BMT. There are now other ways of getting blood stem cells that don’t require bone marrow so the term is more generally called “hematopoietic stem cell transplant” or HSCT. HSCT is used to replace a person’s diseased marrow with a new blood forming and immune system produced from the transplanted donor blood stem cells.
Every patient has different transplant needs based on his or her type of cancer. Stem cell transplants, including peripheral blood, bone marrow, and cord blood transplants, can be used to treat cancers affecting the blood or immune system, such as leukemia, lymphoma, or multiple myeloma.
There are two general types of HSCT used in oncology, autologous and allogeneic transplants.
Autologous HSCT: Uses a person’s own blood stem cells. Auto-HSCT is done so that high doses of chemotherapy and possibly radiation can be delivered and the person then rescued using their own blood stem cells. This approach is not generally used for the treatment of MPNs.
Allogeneic: In allogeneic HSCT, blood stem cells are obtained from another individual who is genetically as close to the patient as possible. This is usually a brother or sister, but may be an unrelated donor who has volunteered to donate stem cells or from frozen cord blood that has been donated. The stems cells are typically collected from the blood, but may be collected from the bone marrow.. The purpose of an allogeneic HSCT is to replace not just the blood forming cells but also to provide an entirely new immune system to the recipient. The immune system from the donor can recognize small numbers of cancer cells and kill them off. The “graft versus leukemia” or “graft versus tumor” effect allows tumors to be completely eliminated when traditional therapies such as chemotherapy, radiation, or targeted agents cannot. However, sometimes this immune attack can become more general and the donor cells attack vital organs. The “graft versus host” effect is often manageable, but can be very severe or even fatal. Additionally, the body can sometimes reject the donor cells and the “graft rejection” can leave the recipient with little ability to make blood cells, which can be a very serious problem. To help prevent graft rejection, patients receiving allogeneic HSCT are typically treated with strong drugs to suppress their immune system, but this can also open the door for infections. Overall, allogeneic transplant is a very aggressive and dangerous treatment for blood cancers. However, sometimes it is the only option that can prolong survival and lead to a cure. If transplant is recommended for you, you will have a full discussion of all of the details related to the risks and potential benefits of HSCT with an expert from our transplant team.
The role of allogeneic transplant in myeloproliferative neolasms has changed over the years. In the past, allogeneic transplant was always recommended for younger patients with chronic myeloid leukemia (CML) in chronic phase. Now, because the CML TKI therapies are generally so effective, allogeneic HSCT is uncommon and restricted to patients who have either not responded to TKI therapy or who have progressed to blastic phase. Transplantation of patients with MPNs such as polycythemia vera (PV), essential thrombocythemia (ET), and myelofibrosis (MF) is highly individualized and generally restricted to those patients who have transformed or progressed to a fibrotic phase or for whom alternative therapy has already failed, who are fit, and who have a suitable donor available. You should discuss with your medical team whether an allogeneic transplant is an option for you.
Blood stem cell harvest: Blood stem cells normally reside in the marrow, but can also be found in small numbers in the blood stream or in umbilical cord blood. Previously, stem cells were always collected from the bone marrow, however, currently it is often preferred to use stem cells from the blood. Drugs can be used to increase the number of stem cells in the blood by drawing them out of the marrow. Sufficient quantities of stem cells for transplant are recovered by circulating large volumes of blood through an apheresis machine and skimming off the portion that contain stem cells. When these stem cells are used for transplant the procedure is sometimes still referred to as "bone marrow transplantation" (BMT), but the term "stem cell transplantation" (SCT) or peripheral blood stem cell transplantation (PBSCT) is now often used. The third source of stem cells is the umbilical cord blood from newborns. The cord is normally thrown away after birth, but contains a small number of stem cells that can be stored and used for transplant.